Some home health agencies are suffering from poor Home Health Compare scores related to assessing fall risk for non-ambulatory patients, while others score in the top percentile. Does the SHP national benchmark reflect actual practice, or an intentional process that agencies are using to deal with the dilemma that CMS has imposed?
No validated or widely used fall risk tool exists for non-ambulatory patients or patients unable to perform the assessment because of physical or mental impairment (Note: Researchers in Connecticut developed a fall risk tool, but it's not available to the entire industry). This dilemma paints agencies into a corner, and they answer "no" to M1910 on OASIS, thus resulting in poor public scores.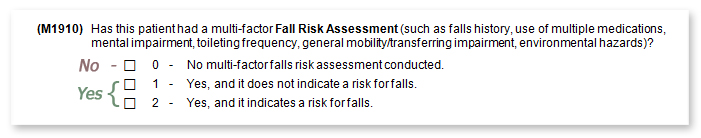
We decided to have a conversation with someone at CMS a few months ago (NAHC has done the same). CMS's response was, "If the patient is bedfast, they're automatically at risk for falls." I don't necessarily agree with that statement, and I'm looking forward to doing further analysis. CMS also told us that non-ambulatory patients don't comprise a large enough portion of home health admissions. Our data indicates that 10 percent (a significant number) of all patients cared for are either bedfast or chairfast, and that doesn't include patients unable to perform the assessment.
Here's where it gets really interesting. Oddly, without a standardized tool, many agencies have superb scores in this metric. Are they primarily caring for patients that are ambulatory? It's rumored that many agencies automatically mark "yes" to M1910 when the patient is bedfast or chairfast. The argument being that the question isn't applicable to the non-ambulatory and the TUG and Missouri aren't validated for these patients. So, why should the agency be penalized. We ran some real-time stats last week on these patients to find out what's really happening in the field.
- 84 percent of agencies responded "yes" to M1910 for bed and chairfast patients.
- 16 percent of agencies responded "no" to M1910 for bed and chairfast patients.
How does M1910 affect the national average for this publicly reported process measure? The score can swing between 86 percent and 95 percent when looking at the same set of patients depending on how agencies complete the question. Since most agencies are responding "yes,” the benchmark is artificially inflated. This penalizes agencies that are responding "no" as directed by CMS. It seems like further clarification from CMS or better industry wide training is needed to ensure accurate reporting on this important preventative measure. Let me hear your thoughts by posting a comment below.