CMS released the hospice proposed rule for fiscal year (FY) 2017 and is seeking public comments through June 20, 2016. The rule updates the typical reimbursement rates and wage index, but includes two new quality measures and a new Hospice Item Set (HIS) 2.0 to collect new data items to support the new measure calculations. CMS also reported that a star rating is coming soon.
The new measures are:
- Hospice Visits when Death is Imminent Measure Pair
- Hospice and Palliative Care Composite Process Measure—Comprehensive Assessment at Admission
With a star rating on the horizon, we can imagine the composite measure would be a straightforward way to calculate a percentile ranking to use in a star calculation. "As the title reflects, the Measure Pair will include two calculations: a) the percentage of patients receiving at least 1 visit from RNs, MDs, NPs or PAs in the last three days of life, and addresses case management and clinical care; and b) percentage of patients receiving at least two visits from MSWs, chaplains/spiritual counselors, LPNs or HHAs in the last 7 days of life. Both calculations are for patients only on the Routine Home Care (RHC) benefit.
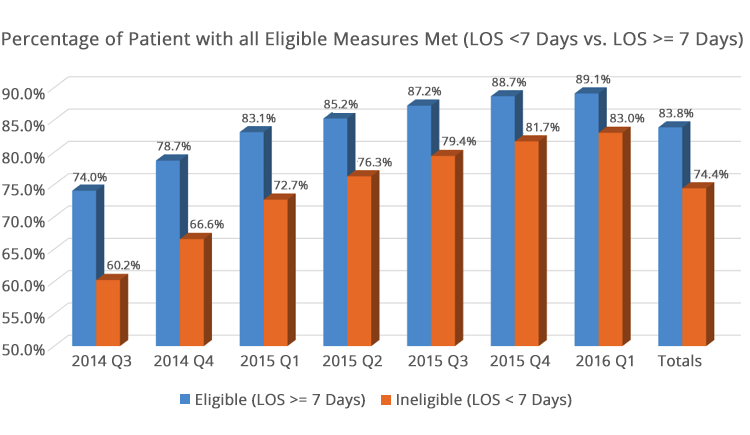
With many of the HIS measures getting close to being topped out, the idea of a composite of all 7 HIS measures seems to make sense. On the graph below, SHP has tracked what this measure would look like for both the eligible patients (at least age 18 and lengths of stay [LOS] equal to or greater than 7 days) and those with LOS less than 7 days.
As we reported at our recent webinar on the Hospice Quality Reporting Program, we have seen all 7 HIS measures improve since the inception of the program, back to July 1, 2014. The composite measure has also improved each quarter over the same period.
With a star rating on the horizon, we can imagine the composite measure would be a straightforward way to calculate a percentile ranking to use in a star calculation. CMS noted in the rule that the Hospice Quality Reporting Program (HQRP) measures will be shared publically in FY 2017 via a Compare site. With a typical quarter or two delay in being able to report on these measures, outcomes as of July 2017 will likely include a rolling 12-month period through either December 2016 or March 2017.
In either case, your scores today will be included in this public data. Hospices should be devoting their time and resources to improving their HIS outcomes, especially as compared to national benchmarks, to be recognized as a high quality “star” hospice.
Another item CMS commented on in the rule was to build a new “assessment instrument,” expanding on the HIS to be able to report on even more quality measures. Although CMS is not proposing the hospice patient assessment tool at this time, I can imagine hospices getting dizzy thinking of what this new workload will mean to them. Seeing stars yet?

