The recently published Medicare and Medicaid CY 2024 Home Health Prospective Payment System Rate Final Rule, documented in the Federal Register on November 13th, solidifies significant shifts in the Home Health Value-Based Purchasing Program (HH VBP) and Home Health Quality Reporting Program (HH QRP). Despite input from industry stakeholders, the Centers for Medicare & Medicaid Services (CMS) held firm on their proposed changes.
A notable addition to the HH QRP is the Discharge Function Score (DFS), introduced to replace the process measure Application of Percent of Long-Term Care Hospital Patients with an Admission and Discharge Functional Assessment and a Care Plan That Addresses Function, where scores had essentially topped out. CMS noted that the performance of the measure is so high it no longer offers meaningful distinctions in performance.
CMS received 50 comments on HH VBP provisions, primarily expressing concerns about adopting the DFS measure. Some argued that any changes to the HH VBP measure-set were premature in view of the efforts agencies have invested in improving performance on the original set of measures.
Within the HH VBP, the DFS will supplant the Total Normalized Composite (TNC) for Mobility and Total Normalized Composite for Self-Care, carrying a slightly higher weight (20.0% vs. 17.5%). The exclusion of the TNC measures from ever being added to the HH QRP suggests they were not intended as long-term measures.
CMS finalized to use CY 2023 as the updated baseline year to evaluate both HHA improvement scores as well as the expanded model benchmark and achievement threshold for this measure and all others. CY 2023 year is almost over, but providers will not know what a “good” DFS score is until CMS publishes scores in the July 2024 Interim Payment Report. CMS does note they will provide agency scores in iQIES as soon as administratively possible and before the start of CY 2025.
In looking at the Abt Associates technical report for the measure calculation, they provided some insight in historical scores based on CY 2021 data where the mean final score among HHAs with at least 20 episodes was 58.0%.
The wide variation across the inter-quartile percentile rankings highlights a performance gap in DFS scores across HHAs as demonstrated in the exhibit below.
Exhibit 4. HHA-Level Distribution of Discharge Function Scores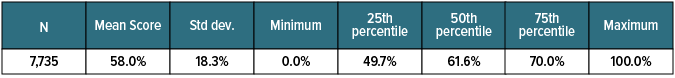
The DFS measure utilizes ten OASIS GG codes for Mobility and Self-Care functions, comparing observed scores at discharge with an Expected Discharge Score derived from risk-adjusting OASIS start and resumption of care responses (SOC/ROC). CMS addresses concerns about patients not improving by acknowledging that "some patients may not be expected to improve" based on risk adjustments.
To address un-attempted OASIS GG-items, CMS will impute a score between one and six using a statistical approach, enhancing precision and accuracy. Considering the increased reliance on GG-items and post-acute care cross-setting reporting requirements, it is likely that this measure will endure. While CMS did not propose changes to Quality of Patient Care Star ratings or Patient-Driven Groupings Model (PDGM) payments using GG-items, the removal of TNC scores may signal a potential shift for OASIS functional items.
CMS continues to align VBP measures with those adopted in the HH QRP measure-set. As the industry adapts, it is crucial for agencies to understand the DFS measure and train staff in accurately coding GG-items. SHP is committed to supporting these efforts by incorporating the DFS measure into its suite of reports next year.
Stay tuned for updates.

