In the Medicare and Medicaid CY 2023 Home Health Prospective Payment System Rate Final Rule, CMS finalized the PDGM permanent behavioral adjustment of 7.85% to be phased in with only half of the rate being adjusted in CY 23. Including the higher revised market basket adjustment of 4.1%, reduced by the productivity adjustment of .1%, CMS is predicting HHAs revenues to increase by 0.7% or $125 million in CY 2023 compared to CY 2022. This compares to the proposed rule where payment rates would decrease by 4.2% or $810 million.
This is good news for sure, but it does kick the can ahead. CMS shared they received 770 comments on the CY 2023 proposed rule compared to 75 comments the year earlier. The behavioral adjustment is based on what CMS assumes as changes in payments not related to patient characteristics in switching the reimbursement model from PPS to PDGM in 2020. CMS does not provide a timeframe for when the other half will be implemented, nor how to address the overpayments from the first three years of PDGM (CYs 2020 – 2022). However, the delay will provide an opportunity for the National Association for Home and Hospice (NAHC) and other stakeholders to better contest CMS’s methodology where they see flaws in the behavioral adjustment calculations.
Another provision in the final rule on the watch list was to see whether the expanded Home Health Value-Based Program (HHVBP) would finalize CY 2022 as proposed, to be the baseline year or revert back to the original CY 2019 baseline year. Comments seemed to be mixed on this change. In the end, CMS relied on comparisons in outcomes from pre-pandemic years vs the first two years of COVID and concluded that 2022 would be more aligned with the performance year’s data under the expanded HHVBP Model.
Since many of the HHVBP OASIS-based applicable measures scores have been improving, the achievement point threshold (median score) for CY 2022 will be higher than if CY 2019 were used. Unfortunately, CMS will not be providing the new CY 2022 baseline year values until the first Interim Payment Reports (IPR) are released in July 2023. Agencies will be blind to what the achievement thresholds and benchmarks will be. CMS’ response in the rule was, “This would be consistent with the rollout of the original HHVBP Model in which benchmarks and achievement thresholds using 2015 data were made available to HHAs during the summer of the first performance year (CY 2016).” I guess what’s good for the goose is good for the gander?
To be fair, CMS noted that before the start of the CY 2023 they would provide agency level HHVBP measure scores and national averages, including the new TNC measures. “To help provide feedback to HHAs, we plan to make the most current HHA specific performance data for the applicable measures available to each HHA in iQIES.”
In the rule, CMS has provided data on how HHVBP applicable measure scores have changed over the last 3 completed years (see chart).
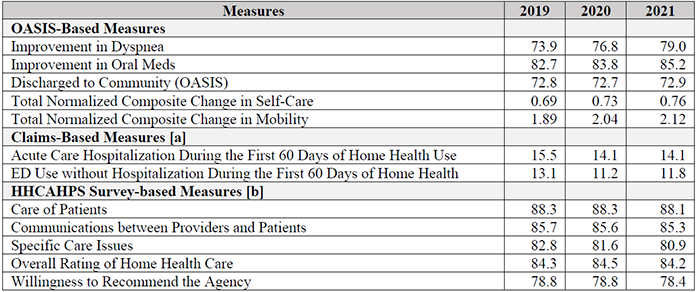
TABLE D2: AVERAGE NATIONAL PERFORMANCE ON APPLICABLE MEASURES (CY 2019 – CY 2021)
OASIS-based measures have continued to improve through the 5-year HHVBP demonstration and into the first two years of COVID, with the exception of the Discharged to Community measure which has remained stable. Claims-based measures improved in 2020 and 2021 compared to 2019, but HHCAHPS scores have been flat with slight declines in 2021 compared to 2020.
With HHCAHPS survey-based and Claims-based measures weighted at 65% of your Total Performance Score (TPS), it will be important to identify opportunities for improvement and best practices within your agencies.
To help our clients, we have teamed up with Berry Dunn to explore the best practice insights that can be gathered by looking at the Berry Dunn National Healthcare at Home study.
Webinar
Please join Lindsay Doak, National Study Director at Berry Dunn and I during our Winning Wednesday Webinar on November 9th at 2:00 ET as we share results from the National Study on the correlations to HHCAHP survey-based and Claims-based measure scores that will help improve your HHVBP performance.

