CMS shared the details of the new Hospice Special Focus Program (SFP) in the CMS Home Health Prospective Payment System Proposed Rule posted in the Federal Register on July 10th. While expected, CMS often adds rule-making for non-home health services when either timing or urgency makes it necessary. Based on the scrutiny Hospice has been under from numerous OIG reports and the negative publicity from articles written by ProPublica and the New Yorker, Hospice has been in the crosshairs of increased oversight.
CMS is proposing to identify the hospices performing in the bottom 10% in the nation and make them subject to the SFP. CMS defines the SFP as a “program conducted by CMS to identify hospices as poor performers, based on defined quality indicators, in which CMS selects hospices for increased oversight to ensure that they meet Medicare requirements. Selected hospices either successfully complete the SFP program or are terminated from the Medicare program.” By posting in the HH Proposed Rule, if finalized, the poorer performing hospices would be identified in Q1 of 2024 based on data available from CY 2023 and prior.
To determine the lowest performers, CMS will calculate an algorithm using data from annual surveys, substantiated complaints and two of the HQRP programs, including the Hospice Care Index (HCI) and four questions from the CAHPS Hospice survey (see chart).
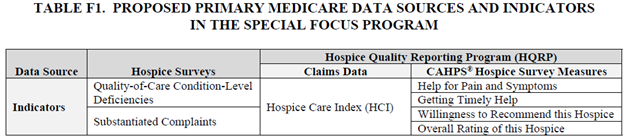
A Condition-Level Deficiency (CLD) is issued when, during a three-year recertification survey, a hospice is found to be noncompliant with all or part of a Condition of Participation (CoP). Of the 23 CoP’s, CMS will use eleven of them in determining the SFP based on the impact they have on patient care. Substantiated complaints will also use a three-year look-back in counting total number of complaints. In the three-year period CMS used to design the SFP, 88.3% of hospices had no CLDs and 81.8% had no substantiated complaints. It makes sense to double-down on preparing for surveys and avoiding complaints given that the results will be used across three years of the annual SFP determinations.
Both the HCI and CAHPS Hospice survey measures are based on 8 quarters of data. For the HCI, CMS notes that 78.3% of hospices had HCI data (for public reporting, hospices with less than 20 claims are excluded). The vast majority of hospices had a HCI score of 8 or better (86.1%).
For the CAHPS Hospice measures, CMS will be using bottom-box scores. I have been so used to looking at top-box scores, I had to revisit what would be considered bottom box. This chart shows the measures, as well as the number and type of responses and that are used in the bottom-box CAHPS Hospice composites.
| Measures listed within | # Responses | Bottom Box Responses |
|---|---|---|
| Help for Pain and Symptoms | Three | No |
| Getting Timely Help; Help for Pain and Symptoms | Four | Never or Sometimes |
| Willingness to Recommend | Four | Definitely No or Probably No |
| Overall Rating | Eleven | Scores of 0 through 6 |
CMS shared in the proposed rule that only about half of all hospices nationally have CAHPS Hospice data. Many are exempt due to the size of their hospices and number of distinct beneficiaries. In scoring CAHPS, CMS will calculate a “Survey Index” where 100 points are awarded for each measure that received a bottom-box score. Since “Willing to Recommend” and “Overall Rating” are considered somewhat similar measures, the scores will be weighted at 50%. A lower the number of points would indicate a higher quality score.
One thing CMS struggled with was how to combine the points for an overall score since each indicator has different units of measure. Survey CLDs and Complaints have no upper limit but the HCI is maxed out at 10 points. CMS is proposing to create a “standardized” score for each indicator by taking the observed values for each hospice, then subtracting from the average score for all hospices. CMS would then divide this number by the standard deviation to reflect the cluster of scores around the average. This essentially creates a magnitude of difference where lower scores would be better.
Since Hospices without CAHPS scores will be missing in the comparison, CMS is also proposing to divide the roll-up score by the number of indicators each hospice will have. CMS plans the weight the CAHPS scores by 2 based on the feedback they received on the importance of these scores from the Technical Expert Panel (TEP) that met on this proposal. With CAHPS data, the calculation would be:
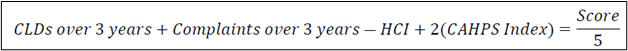
Without CAHPS, the CLDs, Complaints and HCI scores will be divided by 3. These scores would be compared to all hospices, and the providers scoring in the highest 10% (lower is better) would be selected to participate in the SFP.
Once selected, Hospices would only “graduate” from the SFP if, in an 18-month timeframe, the hospice has no Quality-of- Care Condition Level Deficiencies (CLDs) cited or Immediate Jeopardies (IJs) for any two 6-month SFP surveys and have no pending complaints or have returned to substantial compliance with all requirements. If not, these hospices will be subject to being terminated from the Medicare program.
As with many QRP programs, even as hospices work to continuously improve in these indicators, there will always be a lowest 10% of performance. Only by continuing to monitor real-time quality scores and comparing to national benchmarks can hospices stay ahead of their peers and off the SFP list.

