Excited or hesitant, optimistic or worried, hopeful or skeptical? No matter the feelings associated with the Patient Driven Payment Model (PDPM) for skilled nursing facilities (SNFs), the storm will hit on October 1, 2019.
PDPM will drive sweeping changes in the industry and will require a paradigm shift in the way SNFs think about and provide care. To be successful, new tools will be essential to help SNFs optimally distribute resources, achieve desired outcomes, and maximize reimbursement.
Historically we have learned that money talks, with payment structure driving models of care, allocation of resources, and eventually industry norms and ways of thinking. Payment under RUG IV incentivized maximum use of therapies which led to certain industry beliefs that were mostly independent of individual patient characteristics.
PDPM - A new era calls for a new cookbook
Specific details about PDPM can be found on the Centers for Medicare & Medicaid Services (CMS) website. One goal of PDPM is to drive a new model of care based on individual patient characteristics and needs. By removing the therapy thresholds required for higher payment rates, this new model allows SNFs to allocate resources according to the needs of each patient, such as greater therapy for some and more nursing resources for others.
A benefit under PDPM is that resources can be adjusted on a day-to-day basis throughout the stay as the patient’s needs dictate without reimbursement being penalized.
The question under PDPM is how to know the right distribution of services at the start of a patient’s stay and when and how to adjust care to achieve the best functional outcomes while optimizing reimbursement. This requires a new way of approaching care and challenges old ways of thinking.
Think of the process as similar to developing and perfecting a recipe, which requires the right ingredients in just the right amount while controlling variables, such as the right timing and method for adding ingredients and the intensity and duration for cooking. The recipes used under RUG IV were fewer and more straightforward. PDPM is much more complex, requiring a cookbook of recipes that are more sophisticated, allow for individualization, and require a higher level of monitoring and tweaking to achieve the best outcome.
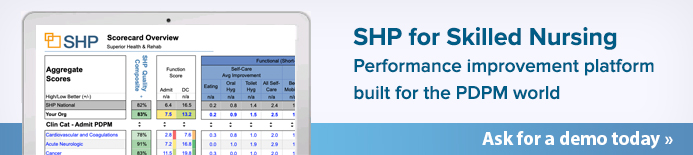
Important to have the right ingredients
To be successful as early as possible in this new era, updated skills and tools are required. Real-time data is a crucial tool as PDPM is much too complex to manage manually. At an individual patient level, information as close to real-time as possible will enable allocation of resources in the right quantity and intensity to each individual patient, including as their status improves or declines. Decisions will need to be made on a near daily basis.
Too many resources in any area creates inefficiencies and wasted dollars, which in turn can negatively impact patient and facility outcomes. Too little of any resource can potentially impact quality and/or create dissatisfaction amongst staff.
The optimal data would:
- be benchmarked against other facilities, providing context for the information
- enable facilities to filter by various patient and setting characteristics, resources provided, and functional outcomes achieved
- provide the ability to drill down to the patient level
However, it is not enough to just have real-time data. The data must also be presented in a meaningful way, enabling the facility to interpret, analyze, and apply the data. The more visually intuitive and easy data is to manipulate, the broader the use of the information by leadership at the corporate and facility level, as well as enabling responsive decision-making by the interdisciplinary team at the patient level.
While implementing PDPM, facility staff will look to leadership for knowledge and direction. Engaging all disciplines and levels of staff in the process is critical in developing a new model of care. Creativity and new ways of thinking must be encouraged and rewarded. It’s important to create a culture that sees unique, individual characteristics of each patient and adapts care and allocates resources to best meet those needs. A culture of efficient use of all resources while optimizing outcomes is a must in order to compete in the changing SNF industry, including adapting to the rising acuity and more complex needs of the patients being cared for in a SNF. Over time, data will confirm the best care delivery “recipes” for optimizing both quality outcomes and reimbursement.